Pituitary adenomas arise from epithelial pituitary cells and account for 10-15% of all intracranial tumors. Tumors exceeding 10 mm are defined as macroadenomas, and those smaller than 10 mm are termed microadenomas. Most pituitary adenomas are microadenomas.
Pituitary imaging is important in confirming the diagnosis of pituitary macroadenoma and also for determining the differential diagnoses of other sellar lesions.
CT scanning is better at depicting bony structures and calcifications within soft tissues than either plain x-ray films or MRI. Differential diagnoses of tumors with calcification, such as germinomas, craniopharyngiomas, and meningiomas, are better determined with CT scanning. CT scans are valuable when MRI is contraindicated, such as in patients with pacemakers or metallic implants in the brain or eyes.
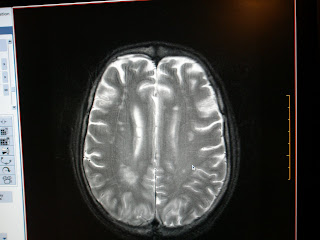
MRI the modality of choice for pituitary imaging because it provides better visualization of soft tissues and vascular structures. No exposure to ionizing radiation occurs. At least a 1.5-T magnet should be used for MRI of the pituitary.
The goal of treatment is complete cure. When this is not attainable, reducing tumor mass, restoring hormone function, and restoring normal vision are attempted using medications, surgery, and radiation. Pituitary macroadenomas often require surgical intervention for cure. The exceptions to this rule are the macroprolactinomas, which usually have an excellent response to medical therapy. Medical treatment can play a role in reducing tumor size, controlling hormonal excess, or correcting hormonal deficiency. Transsphenoidal surgery is the approach of choice. Only about 1% of patients require a transcranial approach. Compared to remission rates of 90% in microadenomas, macroadenomas with significant extrasellar extension have remission rates of 15-37% when treated with surgery alone. Radiation therapy and medical treatment often complement surgery.
For more information on this topic click here